How Menopause Impacts Bone Health: What Every Woman Should Know
Menopause is a significant phase in every woman's life. While it brings with it a host of physical and emotional changes, one of the most profound yet often overlooked impacts is on bone health.
Understanding how menopause affects your bones is the first step to preventing it,
In this blog, we’ll delve into the connection between menopause and bone health, the risks, signs to watch for, and practical steps to keep your bones strong and healthy.
Understanding Menopause and Bone Health

Menopause marks the end of a woman’s reproductive years, typically occurring between ages 45 and 55.
During this period, the ovaries stop producing eggs, and the levels of estrogen and progesterone drop significantly.
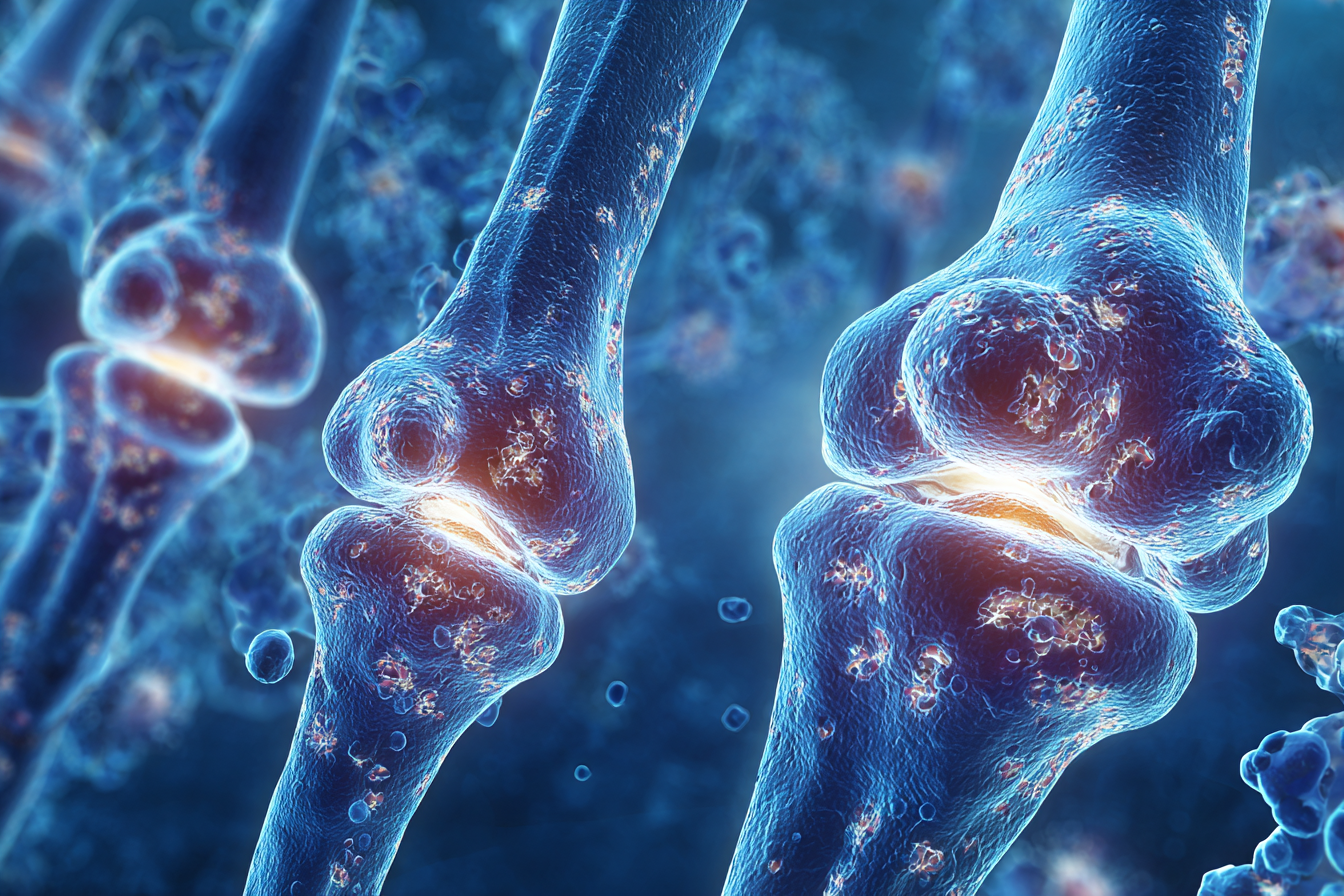
Estrogen, in particular, plays a crucial role in maintaining bone density. When its production declines, bones can lose strength, becoming thinner and more susceptible to fractures.
Why Bone Health Declines After Menopause
Estrogen is a key protector of bone mass. It helps regulate the process of bone remodeling—a balance between bone breakdown (resorption) and bone formation. Before menopause, bone resorption and formation are generally balanced. However, when estrogen levels fall, the rate of bone resorption outpaces bone formation, leading to a net loss of bone density.
This process accelerates in the first few years after menopause. In fact, women can lose up to 20% of their bone density within five to seven years following menopause. This rapid loss increases the risk of osteoporosis—a condition that makes bones porous, fragile, and more likely to break.
Osteoporosis: The Silent Threat
Osteoporosis is often called a “silent disease” because it develops gradually and without obvious symptoms until a fracture occurs. The most common sites of osteoporotic fractures are the spine, hip, and wrist. These fractures can have a significant impact on mobility, independence, and quality of life. Hip fractures, in particular, can lead to serious complications and even increased mortality in older women.
According to the International Osteoporosis Foundation, approximately one in three women over the age of 50 will experience osteoporotic fractures. This highlights the importance of being proactive about bone health, especially around menopause.
Risk Factors for Bone Loss After Menopause
While menopause itself is a major risk factor, several other factors can increase the likelihood of bone loss:
- Family History: Genetics play a role; if your mother or grandmother had osteoporosis, your risk is higher.
- Body Weight: Women with a smaller, thinner frame are at greater risk because they have less bone mass to lose.
- Lifestyle Choices: Smoking, excessive alcohol consumption, and lack of physical activity can all contribute to weaker bones.
- Diet: Inadequate intake of calcium and vitamin D impairs bone health.
- Medications: Long-term use of steroids and certain other medications can accelerate bone loss.
Warning Signs and When to Get Checked
Osteoporosis develops silently, but some warning signs warrant attention:
- Noticeable loss of height over time
- A stooped posture
- Back pain, which could be caused by a fractured or collapsed vertebra
- Fractures that occur more easily than expected
If you are approaching menopause or have already gone through it, talk to your doctor about your risk. A bone mineral density (BMD) test—a painless scan, often called a DEXA scan—can assess your bone health and help guide your prevention or treatment plan.
Steps to Protect Your Bones During and After Menopause
The good news is that there are effective ways to safeguard your bone health:
1. Get Enough Calcium and Vitamin D:
Aim for at least 1,200 mg of calcium daily through food (dairy, leafy greens, almonds) or supplements. Vitamin D helps your body absorb calcium; adults over 50 should get about 800–1,000 IU per day. Sunlight, fatty fish, and fortified foods are good sources.
2. Stay Active:

Weight-bearing exercises like walking, jogging, dancing, and strength training are especially beneficial for bone health. Exercise stimulates bone formation and helps maintain balance, reducing the risk of falls.
3. Avoid Smoking and Limit Alcohol:
Both smoking and excessive alcohol accelerate bone loss. Quitting smoking and limiting alcohol to no more than one drink per day can help protect your bones.
4. Consider Medications if Necessary:
If you have osteoporosis or are at high risk, your doctor may recommend medications that slow bone loss and increase bone density.
5. Monitor Your Bone Health:
Regular check-ups and bone density scans will help track your bone health and catch any potential issues early.
6. Fall-Proof Your Home:
Remove tripping hazards, install grab bars in bathrooms, and ensure good lighting to reduce your risk of falls and fractures.
Emotional Well-being and Support
The changes that come with menopause, including concerns about bone health, can be emotionally challenging. Don’t hesitate to seek support from friends, family, or support groups. Talking to a healthcare provider who listens and understands your concerns is also crucial.
Conclusion
Menopause is a natural phase of life, but its impact on bone health shouldn’t be underestimated.
By understanding the risks and taking proactive steps, you can protect your bones and maintain your independence and quality of life for years to come.
Remember, strong bones are the foundation for an active, healthy future—so make bone health a priority today.